Learning Health Systems
Learning Health Systems: Background
Health care as a complex adaptive system can benefit from data-based guidance regarding issues such as the patient perspectives, locus of decisions, transparency, evidence-based decision making, and waste reduction. This effort aims towards ensuring that every healthcare decision is guided by comprehensive, accurate, and timely health data to improve the delivery of the right care to the right person for the right price [1]. While details surrounding the concept’s operationalisation remain debated, the movement towards value-based healthcare is among the most important yet challenging shifts currently taking place in the healthcare landscape aiming towards achieving the best possible care at the lowest cost. The concept is appealing because it represents a clear strategic focus to guide cooperative efforts to improve healthcare system performance and to potentially align the interests of all stakeholders. The main challenge in search of better value in health is the necessity of significant changes to the way health systems currently deliver and fund care, share data, support innovation, and evaluate performance.
As a first step in the process of development of value-based healthcare system a series of expert meetings were organized by the office of the National Coordinator for Health Information Technology (ONC) and the Institute of Medicine (IOM) of the National Academies. These meeting were organized to explore strategies for accelerating development of the digital infrastructure for the learning health system (LHS). Two. decades ago, in its report, Crossing the Quality Chasm, the Institute of Medicine of the National Academies highlighted the alarming and untenable insufficiencies in health care, noting that every patient should expect care that is equitable, effective, safe, patient-centered, timely, and efficient [2]. In other words, improvement health and economic performance is linked to the success in information technology, computational science, and bio- medical and health research methods. These factors enable real-time generation and application of new knowledge as well as seamless and efficient delivery of best care practices in the context of the of emergence of a learning health system. The pace and progress of the digital transformation will be determined by the alignment of culture, science, and technology, to foster the development of a continuously learning health system. Along these lines, learning health systems (LHS) are healthcare systems in which continual improvement in care is guided by data-based knowledge generation processes are embedded in daily practice. Such a system requires infrastructure, trained professionals, leadership, and vision to flourish.
Based on the determination that health care is a complex adaptive system, one in which progress on its central purpose is shaped by few principles that are simple. In particular, these principles underscore the importance of issues related to the locus of decisions, patient perspectives, evidence, transparency, and waste reduction. Aiming towards development of learning health systems, the IOM report envisioned engaging patients, providers, and policy makers alike to ensure that every healthcare decision is guided by timely, accurate, and comprehensive health information provided in real time to ensure constantly improving delivery of the right care to the right person for the right price.
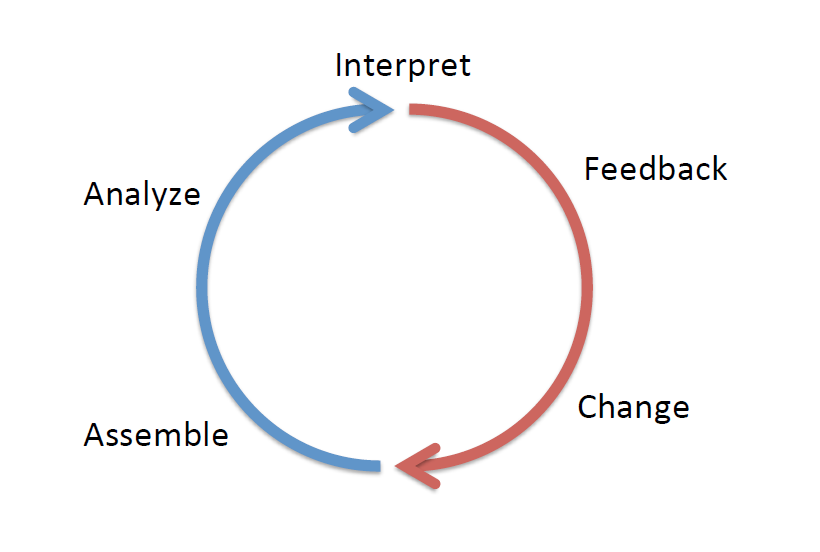
Learning Health Systems are systems in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by‐product of the delivery experience” [3]. More specifically, LHS requires stakeholder involvement to ensure access to robust and comprehensive (meta)data; standardized approaches to analysis; supports for system and practice change at IT and infrastructure levels. LHS’s underlying core values include “accessibility, adaptability, cooperative and participatory leadership, governance, inclusiveness, person focused, privacy, scientific integrity, transparency, and value in healthcare.”[4]
Learning Health Systems: Technologies
Increasing performance of information processing, along with the improved efficiency of the operations that facilitates real-time access to information have spawned new vehicles for progress. In this context existing resources and initiatives actively in play such as telehealth, health information portals, electronic health records (EHRs), personal health records (PHRs), electronic monitoring devices, mobile health applications, and advances in molecular diagnostics are essential part of the LHS digital infrastructure. This adds to the collections of health information repositories, such as biobanks, and health information databases maintained by large health institutes, public health agencies, and private insurers as a blended product of interrelated initiatives arising from within the commercial, independent, and public sectors. Learning health systems will not solely be the result of newly built systems and designed features. There is a rise in the range of newly digitalized services provided by large and small health information vendors. These services are meant to meet the growing demand for capacity to manage the storage, delivery and retrieval, of data for stakeholders in every aspect of health and health care. Moreover, the amount of web-based health information accessed daily by individuals and clinicians, and the frequency with which they turn to the Internet for this information, is already transforming the care process. Along these lines and based on the technologies developed by data giants such as Facebook, Google, and Microsoft, an increasing amount of health-related information available on the Internet.
The array of technologies relevant to the LHS is constantly expanding and evolving including a wide range of health technologies, devices, and IT infrastructure and systems that enables high-quality clinical data to be collected, aggregated, analysed and acted on. A distinct feature of LHSs is the capacity to promote learning as a by-product of everyday care through the use of health data is gathered from electronic health record (EHR) systems, patients’ personal health records and/or research databases or clinical records that collect data used to describe populations with specific diseases or characteristics and monitor their outcomes. Capitalizing on the aforementioned data opportunities the LSH can use machine learning and data mining algorithms to offer a unique capacity to examine trends in care, identify new problems, test solutions, and ultimately accelerate learning and innovation.
capitalising on recent technological advances and based on data flows from routine patient care, LHS aims to enable rapid learning to ensure greater quality, safety and innovation in healthcare. LHSs were defined as systems where “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process and new knowledge captured as an integral by-product of the delivery experience” [5]. LHS is not a unitary and cohesive concept, in contrast, there are many manifestations at different levels. It could be a department that tracks its patient’s outcomes in order to learn and improve its practice. It could be a provider that builds predictive models, from elements of its EHR, which allow it to forecast demand and reallocate resources more effectively. It could be a national distributed network drawing tens of millions of patient records from multiple providers, to assess the effectiveness of particular treatment. Discussions mentioned here represent unique promise for progress and innovation in health care. However, it is noteworthy that the success of LHS projects depends on the achievement of the efforts to create the infra-structure and protocols for enhanced access that are necessary for seamless interoperability.
REFERENCES
[1] National Research Council. (2011). Digital Infrastructure for the Learning Health System. National Academies Pres. Washington, DC.
[2] Baker, A. (2001). Crossing the quality chasm: a new health system for the 21st century (Vol. 323, No. 7322, p. 1192). British Medical Journal Publishing Group.
[3] Budrionis, A., & Bellika, J. G. (2016). The learning healthcare system: where are we now? A systematic review. Journal of biomedical informatics, 64, 87-92.
[4] Menear, M., Blanchette, M. A., Demers-Payette, O., & Roy, D. (2019). A framework for value-creating learning health systems. Health research policy and systems, 17(1), 1-13.
[5] McGinnis, J. M., Powers, B., & Grossmann, C. (Eds.). (2011). Digital infrastructure for the learning health system: the foundation for continuous improvement in health and health care: workshop series summary.